Quick facts about prostate cancer
Prostate cancer is the most common cancer in men in the UK with 1 in 8 men being diagnosed with prostate cancer in their lifetime
More than 52,000 men are diagnosed with prostate cancer every year on average – that’s 144 men every day.
Types of prostate cancer
Almost all prostate cancers are adenocarcinomas – cancers that develop from the gland cells (the cells that make fluid within the prostate).
Other rare types of cancer that can begin in the prostate include
small cell carcinomas,
neuroendocrine tumours (other than small cell carcinomas),
transitional cell carcinomas, and
sarcomas.
Signs and symptoms of prostate cancer
As signs and symptoms for prostate cancer can be similar to other common conditions, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive a prostate cancer diagnosis.
In the early stages of prostate cancer you may not experience symptoms, but as the disease progresses you may experience some or all of the following:

Frequent need to urinate

Difficulty starting or stopping urination

Sudden urge to urinate

Reduced flow of urine

Blood in urine or semen

Lower back pain or pain in the hip area

Unexplained weight-loss

Fatigue
Stages of prostate cancer
The TNM system is used to stage prostate cancer and define what your cancer looks like. The TNM stands for:
Tumour – The degree to which the tumour has affected other tissue
Node – Is a measure of whether lymph nodes have been affected
Metastasis – The degree to which the cancer has spread to other organs of the body
Along with the TNM information, your doctor will also take into consideration your PSA (prostate specific antigen) level from a blood test, as well as your Gleason score to help determine the stage of your cancer. The Gleason score is usually based on the results of a biopsy of the prostate, and it provides an indication of how quickly the cancer will grow and spread.
-
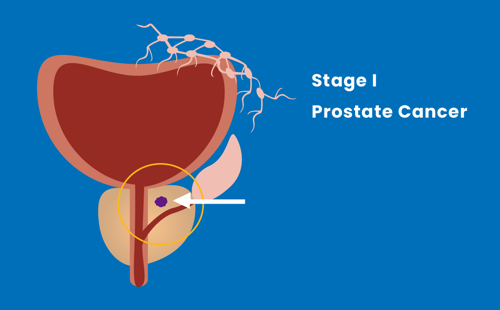
Stage I
The tumour is present in half or less than half of the prostate, and has not spread.
-
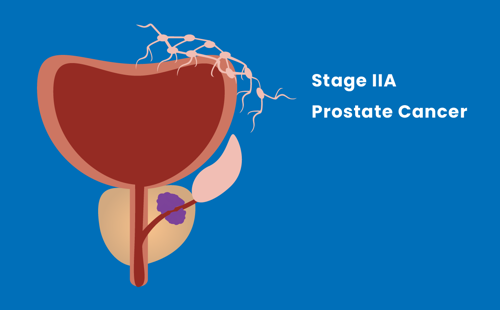
Stage IIA
The tumour may be present in more than half of the prostate, and has not spread.
-
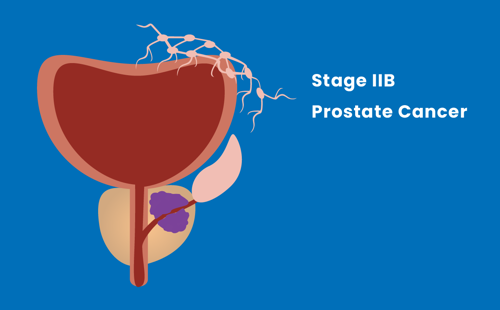
Stage IIB
The tumour has not spread outside of the prostate.
-
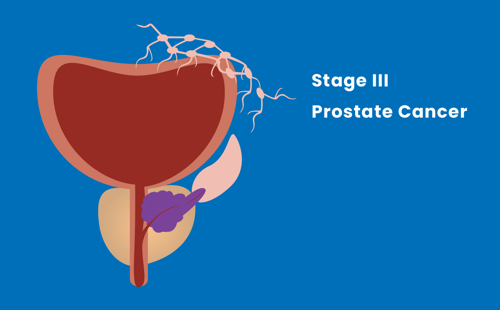
Stage III
The tumour has spread beyond the outer layer of the prostate, but not to lymph nodes.
-
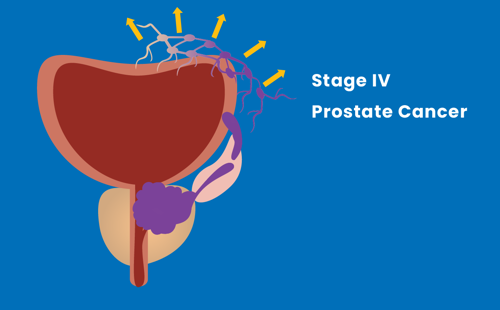
Stage IV
The tumour has spread to nearby tissues, lymph nodes or other organs of the body.
Treatment for prostate cancer
There are many different types of treatment for prostate cancer. Your treatment will depend on you and your cancer.




